Claim Frequency Code 837
Claim Frequency Code 837. In the 837 formats, the codes are referred to as “claim frequency codes.” you can indicate that the claim is an adjustment of a previously submitted finalized claim by using the appropriate code. Providers must submit the claim portion of their appeals first.
Final deadline appeal requests must be submitted with delay reason code 9 in loop 2300 clm20 of the 837 transaction. Adjudicate claims, but will accept the taxonomy code, if submitted. Please note that the use of an incorrect delay reason code will cause.
The Original Highmark Assigned Claim Number Is Required On All Frequency Type Adjustment Claims (Types 7 And 8).
In the 837 formats, they are called “claim frequency codes.” using the appropriate code, you can indicate that the claim is an adjustment of a previously submitted finalized claim. Providers must submit the claim portion of their appeals first. In the 837 formats, the codes are called “claim frequency codes.” using the appropriate code, you can indicate that the claim is an adjustment of a previously submitted finalized claim.
Using The Appropriate Code Will Indicate That The Claim Is An Adjustment Of A Previously Adjudicated (Approved Or Denied) Claim.
The third digit of the type of bill (tob3) submitted on an institutional claim record to indicate the sequence of a claim in the beneficiary's current episode of care. In the 837 formats, the codes are called “claim frequency codes.” using the appropriate code, you can indicate that the claim is an adjustment of a previously submitted finalized claim. For more information, go to edi quick tips for claims.
Adjudicate Claims, But Will Accept The Taxonomy Code, If Submitted.
In the 837 formats, the codes are referred to as “claim frequency codes.” you can indicate that the claim is an adjustment of a previously submitted finalized claim by using the appropriate code. 837 2300 ref payer claim control number is required when clm0503 (claim frequency code) indicates a replacement or void. Values supported for corrections and reversals are:
Frequency Codes Hsn Claims Will Only Be Accepted And Processed Based On The Following Claim Frequency Codes.
4 all dates that are submitted on an incoming 837 claim Please note that the use of an incorrect delay reason code will cause. Healthcare claims status / response.
In The 837 Formats, The Codes Are Called “Claim Frequency Codes.” Using The Appropriate Code, You Can Indicate That The Claim Is An Adjustment Of A Previously Submitted Finalized.
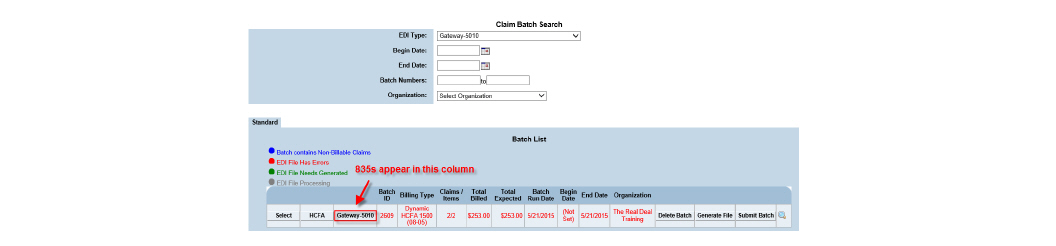
Other electronic transactions you might use. In the 837 formats, the codes are called “claim frequency type codes.” using the appropriate code, you can indicate that the claim is an adjustment of a previously submitted. The original claim number is reported in loop 2300, original reference number (icd/dcn) ref segment.
Comments
Post a Comment